Dr Surinder Sodhi
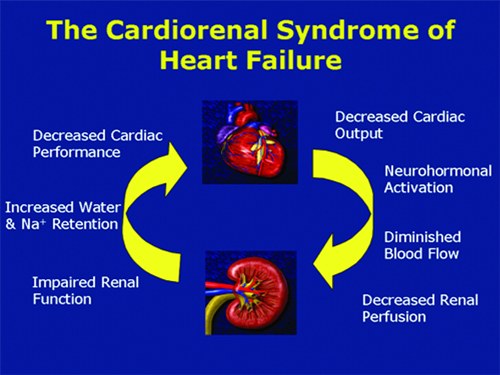
Cardiorenal syndromes (CRS) have been subclassified as five defined entities which represent clinical circumstances in which both the heart and the kidney are involved in a bidirectional injury and dysfunction via a final common pathway of cell-to-cell death and accelerated apoptosis mediated by oxidative stress. Types 1 and 2 involve acute and chronic cardiovascular disease (CVD) scenarios leading to acute kidney injury or accelerated chronic kidney disease.
Types 2 and 3 describe acute and chronic kidney disease leading primarily to heart failure, although it is possible that acute coronary syndromes, stroke, and arrhythmias could be CVD outcomes in these forms of CRS. Finally, CRS type 5 describes a simultaneous insult to both heart and kidneys, such as sepsis, where both organs are injured simultaneously.
The different subtypes and their characteristics are written below in as brief and simple as i can write about it :-
Acute Cardio-Renal Syndrome (Type 1)
This appears to be a discrete syndrome of worsening renal function that frequently complicates hospitalized patients with acute decompensated heart failure and acute coronary syndrome. Many previous attempts to define ‘cardiorenal syndrome’ correspond to this subtype. This entity has specific epidemiology, pathogenesis, treatment and prevention strategies. In our country over 1 million patients are hospitalized each year with acute decompensated heart failure, and estimates ranging from 27 to nearly 40% of these patients will develop acute kidney injury (AKI) as defined by an increase in serum creatinine of 0.3 mg/dl. Those who experience worsening renal function have a higher mortality and morbidity and increased length of hospitalization.
Chronic Cardio-Renal Syndrome (Type 2)
This subtype is a separate entity from acute CRS as it is indicates a more chronic state of kidney disease complicating chronic heart disease. This is an extremely common problem. For instance, in patients hospitalized with congestive heart failure, approximately 63% meet the K/DOQI definition of Stage 3-5 chronic kidney disease (CKD), representing an estimated glomerular filtration rate 60 mL/min/1.73 m2.
Acute Reno-Cardiac Syndrome (Type 3)
Although AKI is recognized as an important cause of acute heart disorder, the pathophysiological mechanisms likely go beyond simple volume overload and hypertension, and the recent consensus definition for AKI will aid in the investigation and analysis of epidemiologic data. The incidence and prevalence of this syndrome are currently unknown but multiple case reports and clinical experience indicate that, in AKI, the heart can develop dysfunction and complications which are predominately secondary to the kidney injury.
Its presence requires the clinical development of AKI as the primary event in a temporal sense, which is then followed by cardiac complications (e.g. hyperkalaemic arrhythmias, fluid overload induced by oliguria or anuria, pericarditis from delayed treatment of severe AKI) all attributable to its presence. In addition, the development of new biomarkers and the study of prevention and management strategies in AKI following radiocontrast or cardiac surgery, for example, should increase our knowledge of how AKI can induce changes in cardiac function. In addition, its definition should allow the specific investigation of how many patients with AKI develop cardiac-specific complications (arrhythmias, pulmonary oedema, infarction) which are attributable to it. This has not yet been investigated.
Chronic Reno-Cardiac Syndrome (Type 4)
A large body of evidence has accumulated demonstrating the graded and independent association between level of CKD and adverse cardiac outcomes. In a recent meta-analysis, an exponential relation between the severity of renal dysfunction and the risk for all-cause mortality was described. Compared with a ‘normal’ glomerular filtration rate of 100 mL/min, the adjusted relative odds for death associated with glomerular filtration rate of 80, 60 and 40 mL/min were 1.9, 2.6 and 4.4, respectively. Overall mortality was driven by excess cardiovascular deaths, which constituted over 50% of the total mortality. This group is not intended to classify all patients with CKD as having a cardiorenal syndrome. Such CKD patients must have evidence of cardiac disease that cannot be attributed to other conditions and where CKD is considered on the basis of history, physical examination and investigations to have contributed to cardiac disease.
Secondary Cardio-Renal Syndromes (Type 5)
Although this subtype does not have a primary and secondary organ dysfunction, situations do arise where both organs are simultaneously targeted by systemic illnesses, either acute or chronic. Examples include sepsis, systemic lupus erythematosus, amyloidosis and diabetes mellitus. The importance and usefulness of defining this syndrome is to allow future investigations of how often there is combined acute kidney and heart dysfunction in patients with some of the above conditions and to facilitate investigations of new diagnostic and interventional strategies which can identify and address common pathways to organ injury. It is acknowledged that this is a controversial addition to the classification and it was widely debated during the consensus conference. Despite its potential heterogeneity, the group considered that the simultaneous presence of kidney and heart disease created a ‘syndrome’ where, on the basis of known pathophysiology, injury to one organ, was likely to, in part, contribute to injury to the other. The group considered that appreciation of such possible interactions may foster the understanding that, under such circumstances, in order to improve the function of the kidney, attention should not be solely directed to it but also focus on how the heart might contribute to it (and vice versa ).
(The author is a Deptt. Of Nephrology SSH Jammu)
Trending Now
E-Paper