Haroon Rashid
Jean and Peter Medawar (1977) rightly said that a virus is “simply a piece of bad news wrapped up in proteins”. An RNA virus with a genome of 30,000 base pairs has effectively brought continents and countries to a standstill, separated States, districts, colonies, even individuals, and delivered a major blow to our economies. We are at war with this virus, and we should fight to win. The aim should not be to flatten the curve; the goal is to crush the curve.
Coronavirus disease 2019 (COVID-19) is an emerging respiratory infectious disease caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), first detected in early December 2019 in Wuhan, China. Till date, more than 4 million individuals have been affected worldwide and causing nearly 2.7 lakh deaths. As on 9th May, 2020, in India, COVID-19 has affected around 63 thousand individuals (836 in J&K) and led to 2101 deaths (9 in J&K). The novel coronavirus has taken just a few months to sweep the globe. It is kind of a perfect storm, difficult to track and control and is severe enough to kill a significant fraction of those who have it.
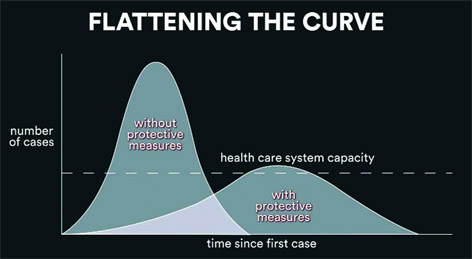
A large number of people becoming critically ill in a short span of time could overwhelm hospitals or health care facilities, resulting in shortage of hospital beds, equipment, or health care providers. There is an urgent need to flatten the curve, by using protective practices, to slow the rate of COVID-19 infection. On a graph, a sudden, drastic increase in number of patients over a short time is represented as a narrow curve with a tall peak. On the other hand, if the same number of patients arrived at the hospital at a slower rate, over the course of several weeks, the line encompassing the curve would be wider, shorter, and flatter. This essentially means that fewer patients would arrive at the hospital each day, ensuring a better chance for the hospital of being able to keep up with adequate supplies, beds, and health care providers for patients. A new disease modelling paper, using data from Ontario, Canada, indicates that dynamic physical distancing, and other measures, could successfully help maintain health system capacity, and prevent intensive care units (ICUs) from becoming overwhelmed because of COVID-19, while allowing periodic psychological and economic breaks from restrictions.
COVID-19 is spreading rapidly, and we only have a few specific tools to control the raging pandemic, and to treat patients. At the moment, we are relying on quarantine, isolation, and infection-control measures to prevent disease spread, and providing supportive care for those who are infected. What we lack is a specific anti-viral agent to treat the infected and, optimally, decrease viral shedding, and subsequent transmission. Modern medicine has so much, yet so little, to offer, when it comes to this pesky little virus. To date, there is no vaccine or specific anti-viral medicine to prevent or treat COVID-19, even as scientists all over the world race to find a cure, or, at the least, a vaccine. Therefore, at present, we only have non-pharmaceutical interventions to rely on. Listed hereunder are the measures that will help in breaking the chain of disease transmission, both locally and globally.
Implementation of public health interventions
Includes bans on public gatherings, closure of schools and non-essential businesses, face mask ordinances, improvement of medical resources, intensive intra-city and inter-city traffic restriction, social distancing, home confinement, quarantine, and cordon sanitaire (i.e., a defined quarantine area from which those inside are not allowed to leave). To stop or slow down the spread of disease, all religious, social and political gatherings, sports events, classes, and festivals need to be cancelled.
Diagnostic tests in sufficient quantities
Not everyone needs to be tested, but everyone with symptoms, and everyone exposed to a symptomatic individual does. Sound medical evaluation, along with early and extensive testing is required. Without rapid diagnosis, the risk of cross-infection in hospitals has been found to be high, and patients are likely to continue infecting family members and close contacts.
PPE:
Personal Protective Equipment (PPE) for health workers and adequate equipment of health care facilities for a surge in number of severely ill patients. We don’t send soldiers into battle without bullet-proof vests; health workers fighting on the front lines of this war deserve no less. Deployment of ventilators and other adequate equipment to hospitals is the need of the hour.
Differentiating the population into severity-based groups and treating accordingly
First, we need to know individuals who are infected; second, who are presumed to be infected (i.e., persons with signs and symptoms consistent with infection who initially test negative); third, who have been exposed; fourth, who are not known to have been exposed or infected; and fifth, who have recovered from infection, and are adequately immune. A separate treatment protocol for each group may then be devised for efficient handling of cases.
Hospitalize only those with severe disease or at high risk
To avoid overloading hospitals, convert hotels/stadiums into quarantine centres to house those who have been exposed. The existing healthcare system cannot afford large numbers of people not strictly requiring hospital care seeking hospital care anyway. Centralized quarantine of patients and close contacts could help reduce in-hospital, local, and community transmission.
In this all-out mission, everyone has to play a role While the mandatory use of face masks by everyone is still a matter of debate in medical communities globally, it can be reasonably assumed that if everyone wears a surgical mask while stepping outside their homes, asymptomatic infected individuals will be less likely to spread the infection to others. Additionally, people who have been exposed recently, and people who are at risk should practice self-quarantine for two weeks, and those who are confirmed to have COVID-19 need to be isolated.
Stay Connected
Social distancing and the anxiety surrounding the exponential growth of COVID-19 cases have affected the mental health of people. While we must practice social and physical distancing, it does not have to lead to social isolation. There is also increased social stigma and discrimination associated with this pandemic that needs to be addressed. A healthy environment needs to be created in which the disease and its impact can be discussed and addressed openly, honestly, and effectively.
[The author is Doctorate (Neuropharmacology) AIIMS, New Delhi]
feedbackexcelsior@gmail.com