Dr Arvind Kohli
 Beating-heat surgery is a way to perform surgery without stopping the heart. The heart continues to beat and circulate blood to heart muscle during the operation. Surgery on a beating-heart helps reduce the risk for complications associated with temporarily stopping the heart during surgery. Now individuals who have medical conditions such as diabetes, history of stroke, or poor physical health, can undergo cardiac surgery with lower risk for developing complications
Beating-heat surgery is a way to perform surgery without stopping the heart. The heart continues to beat and circulate blood to heart muscle during the operation. Surgery on a beating-heart helps reduce the risk for complications associated with temporarily stopping the heart during surgery. Now individuals who have medical conditions such as diabetes, history of stroke, or poor physical health, can undergo cardiac surgery with lower risk for developing complications
Beating heart vs Traditional by Pass Surgery
Beating Heart by pass surgery is different from traditional bypass surgery because it is performed while heart is still beating. Surgeon does not use the heart-lung machine to stop need to use the heart-lung machine during the operation. A prefusionist (a stand by during your operation).
* While not all procedures can be performed on beating heart, with advances in heart support system many techniques have developed that make beating-heart surgery an option for even complex procedures on the inside of the heart including valve repair.
Some of the procedures performed on beating heart include:
* Coronary artery bypass graft surgery (including TECAB, a minimally invasive option performed without cutting the breastbone, as well as open-chest, beating heart bypass)
* Surgery for atrial fibrillation
* Treatment of some congenital heart defects, such as closure of atrial septal defect
* Value repair (mitral, pulmonary, or tricuspid)
* Value replacement (mitral or tricuspid)
Clinical Benefits of Beating Heart Bypass Surgery
Complete recovery from a traditional bypass surgery ranges from four to six weeks. In contrast, recovery time for patients with beating heart surgery has been reported to be as short as three to four weeks. Patients are often awake much earlier after surgery and experience quicker recoveries than patients who have been placed on a heart-lung machine. Hospitalization is generally shorter when compared to traditional operations using cardiopulmonary by pass. Best, of all, the risk of stroke and the need for blood transfusions is substantially reduced with beating heart CABG surgery. The fatty emboli which cause brain damage are generated when the large artery from the heart (aorta) is manipulated and although these are reduced in most off-pump coronary bypass surgeries they are not eliminated because the aorta is still used as site to attach some of the grafts. A growing number of OPCAB surgeons, however, are avoiding the aorta completely, known as “anaoritc” coronary bypass surgery, by taking all their grafts from sites other than the aorta (e.g the internal mammary arteries.) This results in a very low risk of stroke, actually less than occurs during percutaneous coronary intervention.
SURGERY
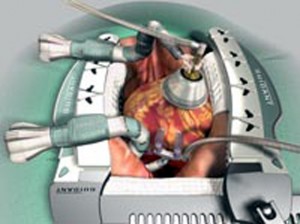
Beating heart surgery, also called off-pump bypass surgery (OPCAB), reduces the risks associated with the use of the heart-lung machine. During a beating heart CABG surgery, the heart continues to beat while the surgeon delicately grafts the bypass. The surgeon uses a stabilization device to still the small area of the beating heart where the bypass is being grafted.
The stabilization device utilizes small suction pods that gently attach to the surface of the heart. The pods work by lifting, not pushing down on the tissue, to stabilize the area where the surgeon will graft the bypass. The device is flexible so that it can be positioned on the heart vessels, yet sturdy so it can steady a portion of the beating heart while minimally affecting heart function.
Beating -heart surgery is technically demanding, requiring specialized skills and training. Therefore, many surgeons prefer not to do surgery on a beating heart. However, since the late 1990s, beating-heart surgery has gained favour among leading surgeons around the world, especially for coronary artery bypass surgery.
Future of Beating Heart Surgery
‘Beating heart’ technology could revolutionize field of heart transplantation. The concept of transplanting a donor heart in a beating state is revolutionary. This promising technology may improve the function of the donor heart, because it remains in a near-physiologic state. It can also help us better assess the suitability of a potential donor.
(The author is Heart Surgeon GMC, Jammu)

