Dr Arvind Kohli
Arterial and venous disease treatment by Endovascular techniques like angiography, stenting, and non-operative varicose vein treatment like endovenous laser and radiofrequency ablation treatment are rapidly replacing major surgery in our country. These newer procedures provide reasonable outcomes that are comparable to surgery with the advantage of short hospital stay (day or overnight for most cases) with lower morbidity and mortality rates. The durability of endovascular arterial procedures is generally good especially when viewed in the context of their common clinical usage like arterial disease occurring in elderly patients and usually associated with concurrent significant patient co morbidities especially ischemic heart disease.
Various conditions which are managed by the vascular specialist include varicose veins, deep venous thrombosis, critical limb ischaemia, Diabetic foot, circulation disorders of the upper limb, aneurysms, carotid disease, hyperhydrosis and thoracic outlet syndrome.
Abdominal aortic aneurysm
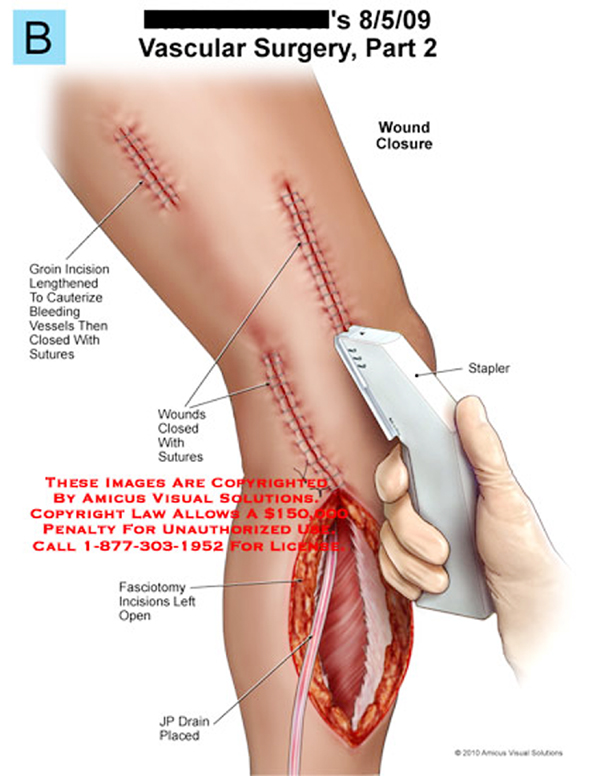
Endovascular repair of abdominal aortic aneurysms was introduced a decade ago. This operation involves radiographically guided intraluminal placement of a prosthetic graft on a wire mesh into the abdominal aorta. This is done via a small groin incision, thus avoiding the morbidity and mortality associated with major open abdominal surgery. As with conventional repair, the goal of endovascular treatment is to prevent further expansion by excluding flow within the aneurysm, thus reducing the risk of rupture. As this method involves less perioperative blood loss and fewer cardiovascular complications, the recovery period is shorter. The procedure can be done under local anaesthetic. The shape of the aneurysm and its relation to other vessels determines suitability for endovascular repair and the type of graft used. However, recognised complications with endovascular repair make the technique controversial. These include graft movement within the aneurysm sac, fracture of the supporting wires, and, the most common problem, endoleak.
Carotid angioplasty and stenting
A minimally invasive alternative to carotid endarterectomy is angioplasty and stenting of a carotid stenosis. However, this carries risks, particularly of cerebrovascular damage secondary to thromboemboli. The use of distal cerebral protection devices is becoming widespread during stenting. These devices are used to prevent plaque debris entering the cerebral circulation. Furthermore, variation in carotid atherosclerotic plaque morphology has been shown to change plaque susceptibility to distal embolisation and subsequent complications. Also, duplex characterization of carotid plaque preoperatively may determine the risk of cerebral complications during carotid endovascular intervention.
Arterial disease in the leg
Most patients with lower limb arterial disease are treated conservatively with statin (Atorvastatin 20 mg once daily) and cilostozol 50 mg twice daily treatment apart from improving peripheral vascular symptoms, it reduced coronary events by 20%. For patients with severe ischaemia, peripheral arterial bypass surgery improves walking distance and quality of life significantly over other approaches.
Minimally invasive techniques are now available to treat lower limb ischaemia. Subintimal angioplasty is a radiological technique in which the angioplasty guide wire enters the extraluminal (subintimal) space within the vessel wall and sissection is done with radiographic guidance. The angioplasty balloon is then inflated within this subintimal space. This redirects the blood flow inside the wall of the artery, bypassing the occlusion, and back into the lumen beyond, leaving the atheroma core in situ with a new channel created around it. The procedure carries a low risk of complications and has a high initial technical success rate. It is used chiefly for long femoral and popliteal artery occlusions in which an intraluminal angioplasty guide wire cannot be passed. Although short term patency rates are excellent, long term patency is not as good as with bypass surgery. The technique may, however, have an important role as first line treatment for patients with both claudication and limb threatening ischaemia and those deemed unfit for surgery.
In some centres, endovascular stents have been used to improve patency after angioplasty in patients with peripheral arterial insufficiency. Often a stent is implanted if the angioplasty result is suboptimal or an arterial dissection occurs or for a restenosis. However, results of short term and long term follow up differ in the literature, overall, stents seem to have little role in treating peripheral arterial disease.
New treatments for varicose veins
Varicose veins are present in upto 40% of the population and are a common indication for surgical intervention, now often done as a day case procedure. Alternatives to the current operative techniques are being introduced to avoid the need for general anaesthesia and to improve cosmetic outcome. Endovenous obliteration using radiofrequency (diathermy) or laser has been devised to close the long saphenous vein, an alternative to the traditional “stripping’’. Another new technique that obviates the need for multiple “phlebectomies” to avulse calf varicosities, thus giving a more cosmetically favourable outcome, is “powered phlebectomy.’’ This minimally invasive approach uses an illuminator under the skin to accurately target the vein, which is removed by suction under direct vision. This leaves the patient without multiple stab incision scars and potentially lowers the risk of postoperative infection.
What the Future Holds
Vascular surgery has come of age over the past two decades. The development of endovascular surgery has been accompanied by a gradual separation of vascular surgery from its origin in Cardiaothoracic surgery. Most vascular surgeons would now confine their practice to vascular surgery and similarly general surgeons would not be trained or practice the larger vascular surgery operations or most endovascular procedures. More recently, professional vascular surgery societies and their training program have formally separated “Vascular Surgery’’ into a separate specialty with its own training program, meetings and accreditation.
As a result of the expanding ageing population and being diabetic capital of world vascular workload in India is showing steep rise and the need for Vascular specialists and Specialised Vascular centres are growing.
Trending Now
E-Paper