Dr Richa Sharma & Dr Amit Basnotra
As such no medical or surgical condition is a contraindication for pregnancy provided its stable and controlled and patient has good survival chances ultimately what is the centre point in an such situation is a healthy mother with a healthy child and the WOC(Welfare of Child)
Liver disease is a rare complication of pregnancy, but when it occurs it may do so in a dramatic and tragic fashion for both mother and infant. Diseases such as acute fatty liver of pregnancy (AFLP) may begin innocuously with mild symptoms and liver enzyme abnormalities but, if left untreated, can progress to jaundice, liver failure, and death.
Pregnancy-related liver disease is the most frequent cause of liverdysfunction in pregnancy and provides a real threat to fetal and maternal survival.
A rapid diagnosis differentiatingbetween liver disease related and unrelated to pregnancy is required in women who present with liver dysfunctionduring pregnancy. Research has improved our understanding of the pathogenesis of pregnancy-related liverdisease, which has translated into improved maternal and fetal outcomes. Here, we provide an overview of liverdiseases that occur in pregnancy, an update on the key mechanisms involved in their pathogenesis, and assessmentof available treatment options.
Correlation with trimester:
Alterations in normal physiological and hormonal profiles occur throughout pregnancy. Moreover, changes in liver biochemical profile are normal in pregnancy.However, up to 3% of all pregnancies are complicated by liver disorders. Severe liver disease, although rare, canoccur and leads to increased morbidity and mortality forboth mother and newborn infant. Liver disorders wereonce thought to be trimester specific, but this is notalways the case. As such, liver disease in pregnancy canbe related or unrelated to pregnancy. Liver diseaseunrelated to pregnancy can be further classified into preexistingdisorders that might become active duringpregnancy and those co-incident with pregnancy.
Anatomical, Physiological, and Biochemical changes during pregnancyMimicing Liver disease-
* A rise in maternal heart rate, cardiac output, togetherwith a fall in blood pressure and systemic vascularresistance, all occur during pregnancy. These alterationsmimic physiological changes in patients withdecompensated chronic liver disease.
* Blood volumeincreases by about 50%, peaking in the second trimester. However, blood flow to the liver remains constant andthe liver usually remains impalpable during pregnancy.
* Telangiectasia or spider angiomas and palmar erythema are normal findings in pregnancy and are caused by thehyperoestrogenic state.
* Gall bladder motility is decreased,which increases the lithogenicity of the bile.
* During a normal pregnancy, serum albumin concentrationfalls due to the expansion in plasma volume,and the alkaline phosphatase activity increases due toadded placental secretion .
* In general, aminotransferaseconcentrations (alanine amino transferaseand aspartate aminotransferase), bilirubin, and gammaglutamyltranspeptidase all remain normal throughout
* pregnancy, and their change should be furtherinvestigated. On light microscopy, the liver appears normal or near normal.
* Ultrasonography remains the safest imaging modalityto visualise the liver during pregnancy. However, iffurther detailed imaging is needed, MRI without contrastis safe. Gadolinium-enhanced MRI should be avoidedbecause of transplacental transfer and unknown effects on the fetus.
Classification of liver diseases in pregnancy
Pregnancy-related liver diseases
* Hyperemesis gravidarum
* Intrahepatic cholestasis of pregnancy
* Pre-eclampsia and eclampsia
* HELLP syndrome
* Acute fatty liver of pregnancy
Pregnancy-unrelated liver diseases
Pre-existing liver diseases
* Cirrhosis and portal hypertension
* Hepatitis B and C
* Autoimmune liver disease
* Wilson’s disease
Liver diseases co-incident with pregnancy
* Viral hepatitis
* Biliary disease
* Budd-Chiari syndrome
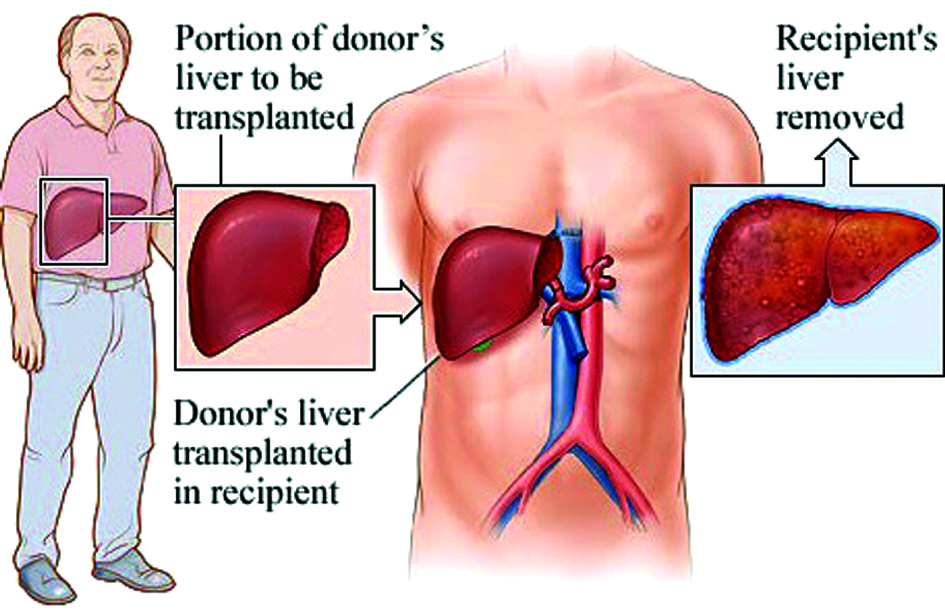
* Liver transplantation
* Drug-induced hepatotoxicity
Multidisciplinary approach to the problem –
Extreme vigilance is needed to detect early signs and symptoms of liver dysfunction and to distinguish these from the anticipated benign hepatic changes of pregnancy. Prompt management can save the life of the mother and the baby. Management of liver disease in pregnancy requires a concerted effort between the primary care physician, liver specialist, obstetrician, and, on rare occasions, a liver transplant team.
Pregnancy Following Liver Transplantation and alternate options:
* With advances in transplantation, and particularly in immunosuppression, it is unnecessary to discourage pregnancy of most female liver transplant recipients at reproductive age
* The first report of successful pregnancy after liver transplantation was published in 1978
* Pregnancy after liver transplantation is often successful, but it must be regarded as a high risk, associated with hypertension, preeclampsia, intrauterine growth retardation, and prematurity. It is best delayed until 1 to 2 years after grafting. Pregnancy planned at least 2 years after liver transplantation with stable allograft function can have excellent maternal and neonatal outcome
* In most female recipients studied, pregnancy does not appear to cause excessive or irreversible problems in graft function if the function of transplanted organ is stable prior to pregnancy, including twins if the woman has stable hepatic function before pregnancy
* In female recipients in contrast to the general population, a high incidence of low birth-weight and prematurity has been a consistent outcome. Immunosuppressive agents may cause hypertension, preeclampsia and renal dysfunction in these recipients.However, there has been no specific pattern of malformation in their newborns or any apparent increase in the incidence of small-for-gestational-age newborns
* immunosuppression during pregnancy is not teratogenic and does not lead to congenital anomalies.
* Nearly 70% of pregnancies after systemic administration of tacrolimus resulted in a favourable outcome without any significant effect on intrauterine growth
* Also, it was found that tacrolimus may decrease the incidence of onset of hypertension and toxemia of pregnancy. Thus, during pregnancy, the female recipient may continue the immunosuppressive regimen to stabilize the transplanted liver function but prevent the effect on the intrauterine growth
* To the present, 37 cases of pregnancies after liver transplantation have been reported worldwide.
* Alternate options available in desparate cases will be- Surrogacy with donor eggs as per the clinical situation.
Conclusion:
Hepatic disorders in pregnancy are rare, but remain clinicallyimportant because of serious adverse effects on bothmother and fetus. Liver disease in pregnancy can presentwith subtle changes in liver biochemical profile or with fulminanthepatic failure. These disorders are complex andmight need to be managed by experienced physicians inspecialisedcentres. Maternal and fetal survival has improvedbecause of better understanding of the pathogenesisof these disorders and higher standards of clinical care
Under careful monitoring a childbearing age woman with stable and adequate liver function may have a successful pregnancy and a delivery after liver transplantation.
( The author are Senior IVF consultant Delhi and Senior GasGastroentrologist Delhi)
Trending Now
E-Paper