Dr Surinder Sodhi
CRRT is a mode of renal replacement therapy for hemodynamically unstable, fluid overloaded patients and patients with sepsis and septic shock in management of acute renal failure especially in the intensive careunit setting. The popularity of ‘slow continuous therapies’ for the treatment of critically ill patients with renal failure is increasing. The techniques which are most commonly used are slow continuous hemodialysis and hemodiafiltration. Slow continuous hemofiltration and slow continuous ultrafiltration also are commonly used.Management in initial hours to counter the derangements in critically ill patients is the most vital thing in the therapy. CRRT initiated for ARF in critically ill patients should serve as a renal ‘replacement’ therapy mimicking as artificial kidney support. It should enhance recovery of the native kidneys with prevention of hyperkalemia, hyper/ hyponatremia, acidosis/alkalosis and rapid correction of pulmonary/ peripheral edema by gradual and consistent removal of extra fluid retained in the body.
Introduction
Intermittent dialysis treatments are treatments that are provided for brief intervals, usually every day or every 2-3 days as required (e.g. intermittent hemodialysis or peritoneal dialysis). Continuous Renal Replacement Therapies (CRRT) are dialysis treatments that are provided as a continuous 24 hour per day therapy.
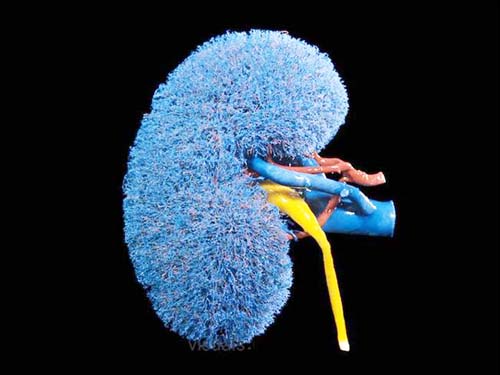
Both intermittent hemodialysis and continuous hemodialysis circuits utilize the same principles. Blood is removed from the patient, pumped through a dialysis filter and returned to the patient following removal of surplus water and wastes. The filter performs many of the functions of the kidney’s nephron unit, hence, it is referred to as an “artificial kidney”.
The major difference between intermittent and continuous therapies is the speed at which water and wastes are removed. Intermittent hemodialysis removes large amounts of water and wastes in a short period of time (usually over 2-4 hours), whereas, continuous renal replacement therapies remove water and wastes at a slow and steady rate. While intermittent dialysis allows chronic renal failure patients to limit the amount of time that they are connected to a machine, the rapid removal of water and wastes during intermittent treatments may be poorly tolerated by hemodynamically unstable patients.
So CRRT is a mode of renal replacement therapy for hemodynamically unstable, fluid overloaded, catabolic septic patients and finds its application in management of acute renal failure especially in the critical care /intensive care unit setting.
The popularity of ‘slow continuous therapies’ for the treatment of critically ill patients with renal failure is increasing. The techniques most commonly used are slow continuous hemodialysis and hemodiafiltration. Slow continuous hemofiltration and slow continuous ultrafiltration also are commonly used.
Advantages
* CRRT by its lower rate of fluid removal can lead to steady state fluid equilibrium in hemodynamically unstable, critically ill patients with associated comorbid conditions eg. M.I, ARDS, septicemia, bleeding disorders.
* It provides excellent control of azotemia, electrolytes and acid base balance. These patients are catabolic thus, removal of urea is mandatory to effectively control azotemia.
* It is efficacious in removing fluid in special circumstances – post surgery pulmonary edema; ARDS etc.
* CRRT can help in administration of parenteral nutrition and obligatory I.V medications like pressors & inotropes by creating an unlimited space by virtue of Continuous ultrafiltration.
* Hemofiltration modality is effective in lowering intracranial tension v/s routine intermittent hemodialysis which can sometimes raise intracranial tension.
*Proinflammtory mediators of inflammation are also shown to have been removed by this modality eg.IL-1, IL-6, IL-8, TNF-a.
Disadvantages
This mode of therapy requires regular monitoring of hemodynamic status and fluid balance (ultrafiltration rate, replacement fluid); regular infusion of dialysate; continuous anticoagulation; ongoing alarms and an expensive mode of therapy above all.
Complications
Technical-1.vascular access malformation 2.Air embolism 3.circuit blood
clotting and decreased blood flow 4.Fluid and electrolyte imbalance.
Clinical- *Bleeding * Thrombosis * Infection/sepsis * Bioincompatibility of membranes * Hypothermia * Nutrient losses.
(The author works in Deptt. of Nephrology SSH Jammu)
Trending Now
E-Paper