Dr. Meeta Gupta
Burden of Disease-Cancer cervix accounts as the fourth most common cancer among women globally, and is the SECOND most common cancer in Indian females after breast cancer. According to GLOBOCAN, about 604,100 new cases of cervical cancer were detected globally and 341,831 deaths were attributed to this malignancy in 2020 alone. It is estimated that 90% of these new cases and deaths occurred worldwide in low and middle-income countries.
In India, cervical cancer accounted for 9.4% of all cancers and 18.3% (123,907) of new cases in 2020. India accounts for the highest number of cervical cancer cases in Asia, followed by China, according to the latest Lancet study on the disease. The research revealed that out of the 40% of the total deaths from cervical cancer, 23% occurred in India, and 17% in China. It is the second leading cause of cancer deaths for females in 12 Indian states, despite it being largely preventable. This situation is specially more alarming in the rural areas where the majority of women are illiterate and ignorant about the hazards of cervical cancer as well as due to scarcity of healthcare resources.
Due to recent advancements in medical science, a powerful tool i.e. Cervical Cancer Vaccination is now available to help prevent this disease. In this article, we aim to raise awareness about cervical cancer vaccination and highlight its importance in safeguarding women’s health. Understanding the benefits and dispelling misconceptions surrounding this vaccine can empower individuals to make informed decisions about their well-being.
In August 2020 the World Health Assembly adopted the Global Strategy for cervical cancer elimination. To eliminate cervical cancer, all countries must reach and maintain an incidence rate of below four per 100 000 women. Achieving this goal rests on the 90-70-90 initiative, and the three key pillars with their corresponding targets:
Vaccination: 90% of girls are fully vaccinated with the HPV vaccine by the age of 15;
Screening: 70% of women screened using a high-performance test by the age of 35, and again by the age of 45;
Treatment: 90% of women with pre-cancer treated and 90% of women with invasive cancer managed.
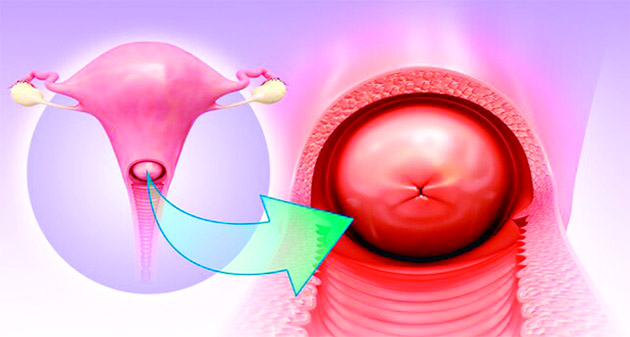
Human Papillomavirus (HPV) infection is one of the major causes associated with this cancer. According to WHO, the HPV vaccine is one of the recommended interventions for primary prevention and is an effective way to reduce the risk of developing this disease. Similar to the COVID virus, Human papillomavirus (HPV) is also a virus that affects millions of people worldwide. It is a member of the family Papillomaviridae. They are small, non-enveloped deoxyribonucleic acid (DNA) viruses. This virus spreads easily from person to person through skin-to-skin or sexual contact. It can spread during vaginal, anal, or oral sex. It is associated with a wide range of health problems, including genital warts and certain types of cancer.
It’s important to note that getting the HPV vaccine does not mean that individuals are free from all risks of developing cancer. However, it does provide an extra layer of protection against the virus, which can go a long way in reducing the incidence of HPV-related cancers. The primary obstacle to HPV vaccination has been financial. Due to the high cost of the available vaccines, it resulted in poor affordability and decreased accessibility to these vaccines. This led to a major hurdle in mass vaccination programs in developing countries like India. However, this is now a thing of the past.
On the occasion of National Girl Child Day this year, the Serum Institute of India launched the first indigenously developed quadrivalent human papillomavirus vaccine (HPV)– “CERVAVAC,” against cervical cancer in women. The vaccine– “CERVAVAC” has been jointly created by the Serum Institute of India (SII) and the Department of Biotechnology (DBT) and BIRAC with the Bill and Melinda Gates Foundation. “It is likely to be priced in the ?200-400 range” as per Mr. Adar Poonawalla, the chief executive officer (CEO) of Serum Institute of India (SII). The vaccine leads to large-scale production of antibodies in the body, thus preventing the virus from infecting cells in the future. The vaccines by themselves are not infectious (the absence of the HPV DNA). However, it should be noted that these HPV vaccines do not protect against other sexually transmitted diseases or treat existing HPV infections or problems.
What are the risks and benefits of the HPV vaccine?
Benefits-The main benefit of getting vaccinated is to prevent certain cancers, including:
* Cervical, vulvar and vaginal cancer in females.
* Penile cancer in males.
* Oral and anal cancer in both males and females.
The vaccine also prevents genital warts caused by HPV.
Risks-The risks, although low, include side effects or reactions to the vaccine. Very few reactions have been reported, but they may include:
* Soreness, redness, or swelling at the injection site.
* Dizziness or headache.
* Fever.
who should not get the HPV vaccine:
* If allergic to yeast.
* Has had a severe allergic reaction to other vaccinations
* Has fever.
* Has had a recent illness.
* Is pregnant or may be pregnant.
Dosage schedule of the vaccine: – WHO now recommends:
* one or two-dose schedule for kids and teens aged 9-14 years
* A one or two-dose schedule for girls and women aged 15-20 years
* Two doses with a 6-month interval for women older than 21 years
* Immunocompromised individuals should receive at a minimum two doses and where possible three doses.
The primary target of vaccination is girls aged 9-14, prior to the start of sexual activity. The vaccination of secondary targets such as boys and older females is recommended where feasible and affordable. Ideally, this vaccine is most effective if given before the start of sexual activity. The vaccine’s effectiveness goes down if it is taken after the onset of sexual activity.
Continued screening importance: Vaccination does not eliminate the need for regular cervical cancer screenings, such as Pap tests or HPV tests. These screenings remain vital for the early detection and treatment of any abnormalities.
Conclusion: Cervical cancer vaccination is a crucial step towards preventing cervical cancer and protecting overall women’s health. It is a safe, effective, and simple way to protect against HPV and its related health problems. By raising awareness about the benefits of vaccination and addressing concerns and misconceptions, we can empower individuals to take charge of their well-being and make informed decisions.
So, if you’re a parent or guardian, consider talking to your doctor about getting your child vaccinated. If you’re an adolescent, consider getting vaccinated to protect yourself and your future. “Together, let us strive to eliminate the burden of cervical cancer and create a healthier future for women worldwide”.
(The author is Associate Dean (Academics) Professor & Head Department of Obstetrics & Gynaecology AIIMS Jammu.)
Trending Now
E-Paper