Dr. Sanjay Sachdeva
Diabetic retinopathy is a condition that occurs as a result of damage to the blood vessels of the retina in people who have diabetes. Diabetic retinopathy can develop if you have type 1 or 2 diabetes and a long history of uncontrolled high blood sugar levels. While you may start out with only mild vision problems, you can eventually lose your sight.
If you have diabetes (type 1 or type 2), you could get diabetic retinopathy, a condition that affects your eyes. But your chances of getting it depend on several things:
The type of diabetes you have
How long you’ve had it
How often your blood glucose changes
How well controlled your sugars are
What causes diabetic retinopathy?
High levels of sugar in the blood over long periods cause diabetic retinopathy. This excess sugar damages the blood vessels that supply the retina with blood. High blood pressure is also a risk factor for retinopathy.
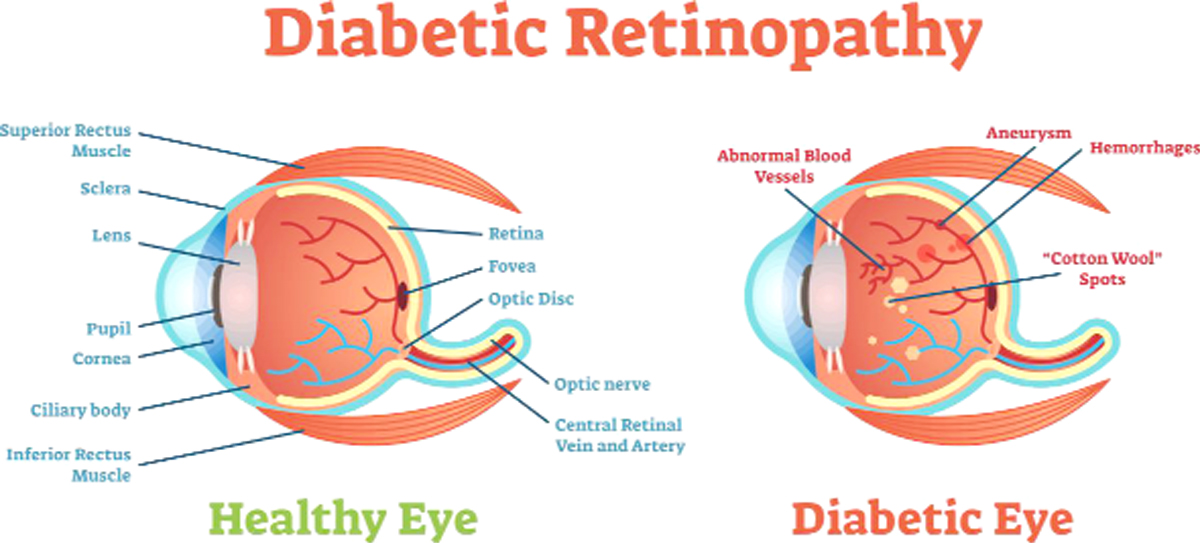
The retina is a layer of tissue in the back of the eye. It’s responsible for changing images that the eye sees into nerve signals that the brain can understand. When blood vessels of the retina are damaged, they can become blocked, which cuts off some of the retina’s blood supply. This loss of blood flow can cause other, weaker blood vessels to grow. These new blood vessels can leak and create scar tissue that can cause a loss of vision.
Risk factors
All people with diabetes mellitus are at risk – those with Type I diabetes and those with Type II diabetes. The longer a person has had diabetes, the higher their risk of developing some ocular problem. Between 40 and 45 percent of Americans diagnosed with diabetes have some stage of diabetic retinopathy.[7] After 20 years of diabetes, nearly all patients with Type I diabetes and >60% of patients with Type II diabetes have some degree of retinopathy;
What are the symptoms of diabetic retinopathy?
It’s uncommon to have symptoms during the early stages of this condition. The symptoms of diabetic retinopathy often don’t appear until major damage occurs inside of the eye. You can prevent unseen damage by keeping your blood sugar levels under good control and getting regular eye exams to monitor your eye health.
When the symptoms do appear, they’re most commonly seen in both eyes and can include:
seeing floaters or dark spots
difficulty seeing at night
blurred vision
a loss of vision
difficulty distinguishing colors
Diagnosis
Diabetic retinopathy is detected during an eye examination that includes:
Visual acuity test: Uses an eye chart to measure how well a person sees at various distances (i.e., visual acuity).
Pupil dilation: The eye care professional places drops into the eye to dilate the pupil. This allows him or her to see more of the retina and look for signs of diabetic retinopathy. After the examination, close-up vision may remain blurred for several hours.
Ophthalmoscopy or fundus photography: Ophthalmoscopy is an examination of the retina in which the eye care professional: (1) looks through a slit lamp biomicroscope with a special magnifying lens that provides a narrow view of the retina, or (2) wearing a headset (indirect ophthalmoscope) with a bright light, looks through a special magnifying glass and gains a wide view of the retina.
How is diabetic retinopathy prevented?
If you have diabetes, it’s important to maintain healthy levels of the following to prevent diabetic retinopathy:
blood pressure
blood sugar
cholesterol
Treatment
Your doctor may recommend laser photocoagulation. It’s a procedure that seals or destroys growing and leaking blood vessels in the retina. It’s not painful, but it might make it harder for you to see color or to see at night.
If your blood vessels leak into your retina and vitreous humor (the jellylike substance that fills the eyeball), you may to have what doctors call a vitrectomy. This procedure removes the blood so you can see better. Without it, you’ll have cloudy vision.
The takeaway
Diabetic retinopathy is a serious eye condition that can lead to diminished eyesight or even blindness in those with diabetes. If your doctor has diagnosed you with diabetes, it’s important to do the following:
Get regular eye exams and physical checkups.
Keep your blood sugar, cholesterol, and blood pressure at healthy levels.
Be mindful of any changes you may notice in your vision, and discuss them with your doctor.
Trending Now
E-Paper