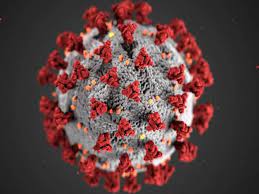
Melbourne, July 7: The SARS-CoV-2 virus was first detected in Australia on January 25 2020. Within two months, the lives of all Australian were upended.
Australians were stranded overseas as external borders were slammed shut. State borders were closed to people from other states. Lockdowns severely restricted movement of the population. People watched in fascination as case numbers went up and then down.
The daily drama dragged on for months, with premiers and chief health officers fronting the media with announcements of case numbers and tightening or loosening of restrictions.
But the daily spectacle made it difficult to see the wood for the trees. Now, new data from the Australian Institute of Health and Welfare shows how Australians’ health changed over the course of the pandemic. It allows us to step back and assess what happened, and to whom.
Australia’s management of the pandemic was overall very good, leading to about 18,000 deaths averted in 2020 and 2021. This was primarily due to restricting arrivals and hotel quarantine for those who did arrive, and lockdowns when quarantine was breached, which inevitable happened.
From late 2021, with more than half the total population vaccinated, these restrictions were lifted following the Morrison government’s national plan, released on August 6 2021.
However, the pandemic is not over. The number of deaths in the eleven months since the plan was released is almost ten times the number than in the 18 months before.
COVID became less deadly, but some Australians were disproportionately affected Australia has had four pandemic waves so far. Daily deaths during the first three waves peaked at around 20 per day. The peak in the current wave is much higher, around 90 deaths per day.
Although more transmissible, the current variant of the virus is less deadly, with a death rate in April 2022 about 0.1% compared to a rate of over 3% in April 2021.
However, the number of daily new infections, some of whom will become long COVID cases, is much higher than in 2021.
Although most deaths throughout the pandemic were in people aged over 60, each of those was a shortened life. Thousands of years of life have been lost prematurely because of COVID.
Deaths did not fall evenly. Those born overseas had twice the death rate of Australian born. The death rate in cities was three to four times that in regional areas.
The bungled management of COVID in residential aged care facilities resulted in deaths in aged care accounting for three-quarters of all COVID deaths in 2020.
The residential age care death rates in 2021 (17%) and 2022 (26%) are tragically high.
People living in the poorest communities had death rates three times that in wealthier communities.
For younger people, COVID was a disease which led to disability rather death, although this does not diminish the impact on those who suffered – and might still be suffering – as a result of the infection or long COVID.
Warnings of things to come
Some preventive care was deferred during the pandemic, which could mean some diseases weren’t detected in their early stages, resulting in poorer outcomes.
Endoscopies are procedures where clinicians look inside the body using a long tube with camera attached, sometimes to detect cancer. Rates of endoscopies were down, suggesting some cancers may have been missed.
This may mean it will be even harder to close the gap between the health of First Nations Australians and the rest of the population.
The overall pattern about mental health is mixed, with raw numbers suggesting no statistically significant change in long-term patterns.
However, there were upticks of reported psychological distress in early 2022, and so the underlying pattern may not yet be clear.
Outcomes have been good so far, but we’re still in the pandemic
Extended border closures led to stress on those separated from their families, and so too did the state border closures. Overall, however, outcomes from the pandemic have been good so far.
But the Australian Institute of Health and Welfare report was released in the same week the 10,000th Australian COVID death was reported. The ongoing deaths from COVID are barely reported in the media and appear to be ignored by policymakers.
The previous prime minister dichotomised potential COVID responses into lockdowns or “living with COVID”. This was never the case.
A more nuanced response – supplementing a drive to increase vaccination rates with mask mandates and density limits when required, and improving ventilation – was always part of the public health response.
Unfortunately, third dose vaccination rates are sitting at around 70% of those eligible, leaving many Australians dangerously exposed to the virus.
There should be a return to the “vaccine-plus” strategy, where we focus on lifting vaccination rates and implementing other public health measures – such as mask mandates or density limits – where required.
Otherwise we risk all the good work done in 2020 and 2021 being completely negated and more unnecessary deaths occurring, especially among the most disadvantaged. (The Conversation)
(AGENCIES)
Home International How has COVID affected Australians’ health? New report shows where we’ve failed...