G V Joshi
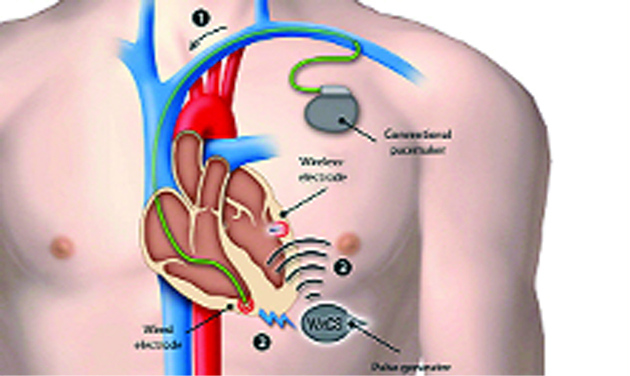
Dr Vivek-Reddy Mount Sinai Hospital, USA has implanted the first miniature-sized, leadless cardiac pacemaker directly inside a patient’s heart during a catheter-guided procedure through the groin via an artery.
It resembles a small metal silver tube, and is only a few centimetres in length, making it less than ten per cent the size of a traditional pacemaker.
The device, is being tested for safety and efficacy in an international, multicentre clinical trial. This research trial will be testing the latest innovative, non-surgical pacemaker for patients experiencing a slowed heart beat. This new-age, tiny pacemaker may ultimately be safer for patients because it doesn’t have leads or has not to be inserted under the skin of a patient’s chest, like a traditional cardiac pacemaker.
Similar to other commonly used cardiac pacemakers, the new device treats a heart rate that is too slow called bradycardia in medical jargon.
It works by closely monitoring the heart’s electrical rhythms and if the heart beat is too slow it provides electrical stimulation to regulate it. The possible advantages of the leadless pacemaker include the elimination of a surgical pocket and no visible pacemaker device under a patient’s chest skin, no incision scar on the chest, no connector wires or leads, and no restrictions on a patient’s activities.
The device’s benefits may also allow for less patient discomfort, infections, and device complications and dysfunction. In addition, the freestanding, battery-operated pacemaker device is designed to be fully retrievable from the heart.
Pacemakers with leads are being manufactured in India by Shree Pacetronix Ltd. As of today a few thousand special pacemakers are being imported. With rising aging population, the demand is likely to go up.
The pacemaker is an electronic cardiac-support device that produces rhythmic electrical impulses that take over the regulation of the heartbeat in patients with certain types of heart block caused by drugs, heart surgery, and more often, simply due to old age.
The normal rate of 72 to 80 beats per minute may go down drastically. The heart may often stop beating for brief periods. The pacemaker sends the life giving electrical signals to such faltering hearts without any interruption, without which most of the victims would die within a few minutes.
In a normal healthy heart, a small network of fibres called the natural pacemaker situated at the top of the right auricle shoots out a rhythmic pulse of electricity 72-80 times a minute. These pulses trigger the muscles in the upper chambers of the heart causing them to contract.
Then after a fraction of a second, the whisper of electricity is passed along the ‘Bundle of His’ (pronounced hiss), another minute collection of nerves and muscles, named after German physiologist, Wilhelm His. The electrical discharge spreads to contract the ventricles, which pump blood to the arteries that keep a human being active and alert. When the natural pacemaker is damaged due to disease or old age, the heart begins to ‘miss.’ It slows down to a dangerous level of 20 or 30 beats a minute. At this low level, the kidneys get insufficient blood and fluids start accumulating in the body.
The brain goes slow and in severe cases the heart stops beating resulting in fainting and blackout. The outlook for such patients was rather grim before 1950 and most of them passed away within a few months. In 1952, Dr. Paul Zoll of the US developed an artificial external pacemaker, which sent sharp impulses of electricity through the chest to the heart.
The instrument worked but occasionally it caused burns. Many patients were afraid of the electrical shocks at such a fast rate of 72 per minute.
An American heart specialist Clarence Lillehei born in 1918, a heart block patient himself, thought of rewiring damaged hearts by hooking electrodes to them and connecting the wires brought out of the body to an external pacemaker. With such a direct connection, a mild shock of 3 to 4 volts was sufficient to produce the desired effect.
In October 1958 Dr. Lillehi began installing his device. Arne Larsson, now 83 became the world’s first recipient of the external pacemaker. But life shrank to the distance covered by rolling beds and extension cords. The spot where the wires came out of the body got infected at times. They were a nuisance while bathing or exercising.
By this time the long lasting button cell batteries we now use in watches and calculators were ready.
Wilson Greatbatch, an electronic wizard working with a heart specialist Dr. Chardack of the US thought about a pacemaker equipped with such batteries, which could be implanted within the body.
The electrical circuitry and the battery were all packed into 150 gm plastic packs. Only the electrode well insulated except for the tip came out of the device. It was introduced into a large vein and from there into the heart, usually the upper-right chamber.
The first model was ready soon. The circuit comprised of a pulse generator, was inserted under the skin of the shoulder or abdomen and delivered minute regular electrical impulses, at 3-4 volts. These impulses stimulated the heart muscle to contract, thus regularising the heartbeat to normal 72 beats a minute.
The gadget was first tried on a dog and was found to be working. On April 15, 1960 Dr. Chardack came across a 77-year-old heart block patient who would live for a few months only. After implanting the pacemaker, life returned to normal. He lived for another 30 months until his old and tired heart gave out. One pacemaker was implanted in Larsson’s body and since then Larsson has undergone 25 surgeries to install implantable pacemakers that failed or had to be changed due to dead batteries. Technical advances have progressively reduced their size and increased the life of batteries that power them to ten years. Some batteries made of lithium last up to 12 years. Some models can automatically provide for a slower heart rate while resting or sleeping.
The microprocessor senses when the pacemaker needs to operate and can be adjusted by an external programmer – similar to a small computer – transmitting radio frequency signals.
Once in place, the electrode and wires of the pacemaker usually require almost little or none attention. The power source of the implanted pulse generator, however, requires replacement at regular intervals depending upon the life of the battery.
If the trials of the leadless pacemaker in the US are successful, it should be manufactured in India. It will bring down the cost of implanting considerably.
Trending Now
E-Paper