Dr. Yash Pal Sharma
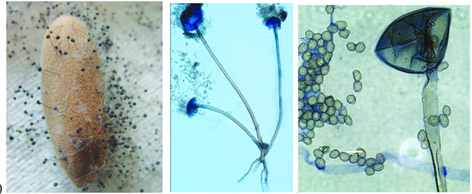
After a momentary respite in late-2020 till February 2021, the transmission of the Systemic Acquired Respiratory Syndrome Coronavirus-2 (SARS-Cov-2) reached unprecedented levels around the world and more particularly in India as people are once again grappling with the ferocity of the second wave of this ever-mutating retrovirus grievously affecting both rich and poor, all ranks and professions, class and creed, regions and religions, urban and the rural, and across all nationalities irrespective of borders and boundaries. And now, as if the scary wave of the deadly virus was not enough, the medical complications of Mucormycosis are on a rise in the Indian subcontinent. In general, mycosis refers to a comprehensive invasion of living cells, tissues or organs in humans and animals with the physical presence of fungal propagules such as spores or hyphae at the infection site. Mucormycosis, a rare but dangerous fungal infection of the sinuses, the brain and the lungs caused by the members of the order Mucorales (of the class Mucoromycetes, subphylum Mucoromycotinaof the Phylum Zygomycota). The fungi most commonly associated with human mucormycosis include Mucor circinelloides, Rhizopus arrhizus, R. microsporusand Rhizomucormiehei, while Syncephalastrumracemosum, Cunninghamella bertholletiae, Apophysomyces variabilis, Lichtheimiaramosa, andSaksenaeavasiformisare less commonly implicated in human mucormycosis.
All these fungi are cosmopolitan, ubiquitous, predominantly saprophytic soil, and air-borne but are of opportunistic behaviour. I vividly remember that while doing our research studies on the mycoflora of various food and agricultural studies as well as during practical demonstrations to post-graduate students (MSc. Botany) in the mycology class practical with common Mucorales genera like Mucor, Rhizopus (bread moulds), Syncephalastrum, Circinella, etc. it always used to be an exciting experience and was never scary.
But the recent unanticipated, distressful emergence of life-threatening mucormycosis in severe and critically ill COVID-19 patients. has taken everyone by surprise. A number of mucormycosis related fatalities from Maharashtra, Gujarat, Rajasthan and other regions of the country and now the first case of mucormycosis on May 20 2021 from the Jammu region of UT of J&K in a highly compromised post COVID patient on steroid therapy, have given us many reasons to ponder that what and where did something go wrong? Although, the primary route of infection is the inhalation of the spores of these fungi, yet all of us wouldn’t catch the infection but weak and immunocompromised would probably do. The majority of the cases of mucormycosis are not occurring in the active phase of COVID-19 but develop as post-COVID-19 complications. This has raised serious concern both for medical mycologists and healthcare professionals. The challenge seems to be bigger since mucormycosis, if not controlled, can further augment the susceptibility of infected patients to more fatal systemic pathogenic infections.
India ranks first with the highest cases of pre- COVID-19 mucormycosis with the prevalence of approximately 0.14 individuals per 1000 population, much higher than the worldwide estimated rate for mucormycosis. Of the various types of mucormycosisviz., rhino-osteo-cerebral, pulmonary, cutaneous, gastrointestinal and others, pulmonary mucormycosis is the most common clinical manifestation. The main predisposing factors of this type of multiple trauma include lifestyle ailment of Diabetes mellitus, an increasing number of immunocompromised individuals with carcinomas and HIV/AIDS, unabated, unethical and rampant use of antibacterial and antifungal drugs, burns, wounds, malnutrition, poor hygiene, poor ventilation, ageing, and intravenous drug abuse. And now the COVID-19 patients that is put on steroids.
A lot of information and views are expressed in health bulletins and social media to curb the menace of mucormycosis. However, basic hygiene and sanitation remain the key. ‘Nip the Evil in the bud’ should be the course of action. Aeromicrobiological monitoring in and around the hospitals, better indoor air quality, cleanliness of contaminated air-conditioning systems, sanitation of the oxygen-generating filling units and cylinders etc. need immediate and regular attention by the households, industrial units as well as the health administrators at the institutional front. The intervention of health professionals can then further prevent the mucormycosis by the early diagnosis, recommending an appropriate antifungal therapy, surgical removal of infected tissues or non-vital organs, However, the early and proper etiological diagnosis, epidemiology, and the susceptibility of humans to these infectious agents and availability of rapid and effective therapy against varied mycoses are the serious challenges confronting all of us.
Although the research related to quick, reliable, and cost-effective diagnostics is going on a war-footing scale, currently, the diagnostics are mainly dependent on mycological (fungal) identification and histopathological examination. Recent breakthroughs in human and fungal genomics has produced several promising targets for novel therapeutic interventions and hopefully, the global convergence of human resource, technology innovations and economic resources would pave way for possibilities to improve human health and a better future. Nevertheless, sanitation and ventilation, balanced nutritional behaviour, appropriate consumer and environmental behaviour, increased public awareness of fungal infections is primarily critical to developing prophylactic and preventive strategies for the effective management of various mycoses including mucormycosis.
We must understand that all diverse organisms including viruses, fungi and humans have a specificity of habitat, the environment in which they grow, the ecological role they play, and the survival strategies they develop. Therefore, because of our ignorance and callousness, creating new environments and habitats for these organisms can certainly disturb their behaviour thereby letting a simple ailment resulting in an epidemic and finally into an uncontrollable pandemic. This exactly seems to be the reason presently for the hostility and aggressiveness of these opportunistic fungi against humans. Therefore, play your role NOW, and remember, ultimately believing and fostering trust in basic science is a must for alleviating human sufferings. So let’s believe in Science while remembering the Divine.
(The author is Professor & Former Head, Department of Botany University of Jammu, Jammu)
feedbackexcelsior@gmail.com
Trending Now
E-Paper