Dr. Kasturi Lal
Urethral narrowing and stress urinary incontinence are two leading pathologies in elderly women .These leading pathologies remain under recognized. Both pathologies have different set of symptoms, underlying causative factors and module of treatment. Thus it would be pertinent to discuss each pathology individually relating to their origin with the process of ageing.
The process of ageing
By reviewing both modern and historical data it becomes apparent that the age at which cessation of menses occurs has not appreciably changed in the past several hundred years. Individual genetic traits have their life span beyond the climacteric. The life span of human is substantially more than other genetic traits. We can now anticipate the average women to live 1/3rd of her life beyond the menopause. During post climacteric years of a woman’s life the impact of loss of ovarian hormone is felt. Marked changes are noted to occur in reproductive failure and increasing incidence of diseases of urethra. To combat the medical problems associated with climacteric a better understanding of the general consequences of ageing as well as those aspects attributable to the loss of gonadal function will be required. This should provide a marked improvement in the quality of life for the expanding elderly population with an emphasis on the prevention of symptoms attributable to a lack of ovarian hormone. Urethral narrowing and stress urinary continence to a great extent are attributed to ovarian hormone deficiency.
The urethral narrowing
The urethral symptoms in elderly patients without any anatomic lesion in the absence of any urinary tract infection has drawn recently the attention of gynaecologist.The combination of painful micturition without any demonstrable lesion has been called the urethral syndrome . Urethral narrowing has been well recognized in elderly women suffering from urinary disturbances such as dysuria and acute retention.
Pathology
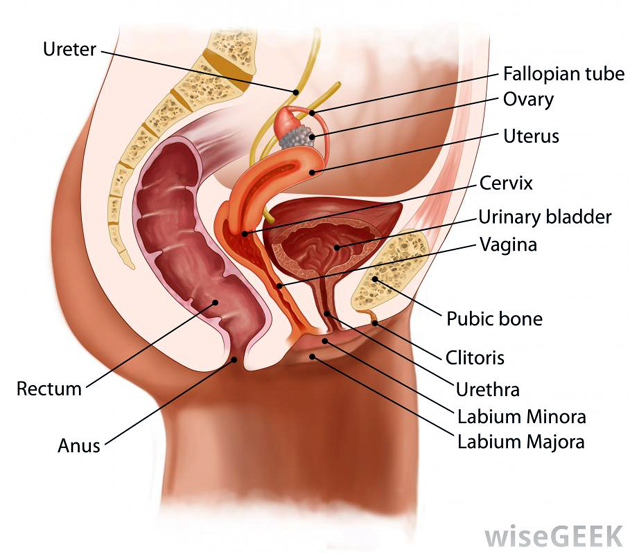
With reduced estrogen the lining of vagina gets thinned .This effect may be followed clinically by dyspareunia and increases susceptibility to trauma and infection. Similar changes have been noted in the urethra and trigone of the bladder where estrogen receptors have also been identified. When such urethral atrophy occurs patient may develop the urethral syndrome with consequent dysuria, frequency and urgency of urination, nocturnia and post void dribbling. There is marked variability in the onset and severity of atrophy of the urogenital tissues. This is in part due to variations in the rate of decline of estrogen production which may be acutely or chronically muted by factors that increase either pre hormone production or efficiency of conversion of prehormone to estrogen. Some women may become symptomatic in months, other take years to show symptoms of urogenital atrophy and some never develop such symptoms.
Symptoms and Signs
The symptoms are wide and varied. The patients present with vague gastrointestinal, nervous, musculoskeletal disturbances besides the urinary problems. The urinary disturbances are frequency urgency and even bouts of incontinence. In some cases patient have to wait and strain to pass urine. The high degree of obstruction with renal damage and hydronephrosis has been demonstrated. There are extreme cases that have marked degree of chronic retention of urine.
Treatment
The epithelium in the distal part of urethra has been found to correspond with vaginal mucosa of squamous variety. This epithelium responds to estrogen. When urethral narrowing is related to atrophic urethritis estrogen should be used for treatment along with the surgical procedure of dilatation of urethra.
Challenges
What worries us more is the limited knowledge of many aspects of urethral disease. There is lack of awareness of urethra in the mind of many gynaecologist . Far too many clinicians choose to ignore this short canal being pleased to regard its symptom as a mere expression of neurosis. There is a lamentable ignorance about the urethral symptoms without any definable disease .The personal misery and the social disruptions which are causes by urethral disease deserve more sympathy. It is suggested that clinician should avoid referral of such patients from surgery to urology to psychiatry clinic. They should plan treatment with good humor and their results would be gratifying.
Stress Urinary Incontinence
The unintentional release of urine during normal everyday activities is a condition affecting millions of women around the world. It occurs when the urethra the tube through which urine exits the bladder is not functioning systematically. When pressure is put on the bladder the urethra cannot put a tight seal to prevent involuntary urine loss. A recent study conducted on women living in urban areas revealed that 50% of females between the ages of 20 to 70 years leak urine at least occasionally. The incidence of regular leakage on strain increases with advancing age. There is a significant observation that 9% of 40 years old women and 19% of 60 year old women report incontinence more often which require treatment.
Pathophysiology
Urethral sphincter maintains a sustained and constant pressure which is unaltered by coughing and straining. But if the sphincter becomes damaged or weakened or lost by some process incontinence occurs after a slight rise in the abdominal pressure .The incontinence occurring due to pure weakness of the intrinsic sphincter is called intrinsic sphincter deficiency and is classified as type III Stress urinary incontinence. Women remains continent as long as the proximal urethra remains above the pelvic floor and the flutter valve mechanism closes the urethra at the time of stress. If however the support of the bladder neck is damaged the proximal urethra may descent below the pelvic floor during strain and the flutter valve mechanism will not act on the urethra resulting in urinary leakage. This is called the hypermobility of the urethra an classified as type II stress urinary incontinence. Pelvic floor dysfunction is the main reasons behind the symptoms of stress urinary incontinence. The anatomical changes are caused by the child birth or damage of pelvic floor structures. Impairment or disorganization of collagen function is causing disruption of elements necessary to maintain anatomical structures involved in the closure mechanism of the urethra. These elements are ligaments, muscles and the vaginal supports of the urethra. Multiparity, obesity and chronic cough are usually associated with disability.
Treatment
Many surgical procedures have overcome the incidence of failure and improved compliance. A dedicated team offers new surgical solution such as TVT and TOT to meet challenges in the years ahead. We have developed the logistics of real operative approach to stress incontinence. The surgical procedures are feasible cost effective and can be integrated in the health care delivery system.
Complex issues
Patients in developing world do not consider this disability worth medical attention, even if the social and psychological impact and effect on quality of life is crucial. It is a great challenge to the physician to deal with the patients who seek therapeutic option. The individuals perception of suffering is variable. An inactive woman using pad permanently may describe her incontinence as not bothersome while an active woman in profession even with occasional leak can feel the thought of leakage devastating. Between these extremes lie all varieties of coping and adaptation of lifestyle in face of these sobering realities new surgical options must be used to address the complexity of managing stress urinary incontinence.
(The author is Director, Institute of Obstetrics And Gynaecology, Kunjwani Bye Pass , Jammu)
Trending Now
E-Paper