Dr. Ajay Anand
Kidney stones occur in 10% patients in their lifetimes. More than 10 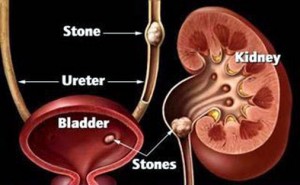 crystal types have been reported. A reversible metabolic abnormality is seen in more than 90% patients. Targeted medical therapy is necessary to prevent growth of pre-existing stones & new stone formation.
crystal types have been reported. A reversible metabolic abnormality is seen in more than 90% patients. Targeted medical therapy is necessary to prevent growth of pre-existing stones & new stone formation.
Urinary stones arise due to:-
* Crystallization.
* Aggregation of supersaturated ion complexes in urine
Different crystals precipitate depending on urine pH, volume, calcium, citrate concentration etc. Therapy has therefore to be tailored as per stone composition and 24-hr urine results. Possible 24 hour urinary clues to diagnosis of stones include elevated urinary calcium, oxalate and sodium levels; decreased urinary volume and citrate levels.
Different stone types include:-
* Calcareous stones (75%)
Ca oxalate, Hydroxyapatiten and Brushite
Medical therapy in these targets physiochemical defects as hypercalciuria, hypocitraturia, hyperoxaluria and low pH of urine
* Nonclacareous stones (25%)
Struvite, cysteine, uric acid
Medical treatment in these type of stones include chemolytic agents, cystine binding compounds, bacterial urease inhibitors
Though surgery is the mainstay of treatment for management of urinary stones, metabolic evaluation and medical treatment of abnormalities noted are strongly indicated in stone patients especially patients with history of lithuria (stone passers), recurrent stones, bilateral stones. In addition to serum and 24 hour urine metabolic work-up, ultrasonogram of neck and serum parathormone estimation are indicated in such patients to exclude parathyroid adenoma and hyperparathyroidism.
Stepwise approach in medically diagnosing patients with stones includes:-
Step I
* History and minimum diagnostic tests
Step II
* 24 hour urinary stone risk profile (customary diet)
* Identification of abnormal dietary factors
* Short term dietary modification
Step III
* Repeat stone risk profile after dietary modification
Step IV
* Elucidation of causes and construction of treatment options for abnormal risk factor
Figure: – Complete staghorn calcululus Left kidney
Fluids:-
Adequate fluid intake prevents urine stagnation and formation of symptomatic calculi. An intake of 3 litre per day is required to produce urine output of 2 litre per day.Nine 10-oz glasses of water or other beverages/day (2700 ml) is must, assuming that one glassful of water is contained in solid food.
Desired fluids include-
Potassium-containing Fruit juices
* Orange
* Grape fruit
* Cranberry
Citrate containing soft drinks
They exert citraturic action by conferring an alkali load.
Less desired fluids include-
* Tea (High oxalate content)
* Milk (High calcium content)
Consumption of lemonade -120 ml conc. lemon juice (5.9gm citric acid) mixed with 2 litre water/day for 1 week increases citrate excretion by 204 mg/24 hrs and decreases stone formation rate from 1to 0.13.
Orange juice like K citrate decreases urinay undissociated uric acid, increases inhibitor activity (formation product) of brushite. Orange juice is beneficial in control of calcareous and uric acid nephrolithiasis.
* Soda flavoured with phosphoric acid may increase stone risk, whereas soda with citric acid may decrease risk
* Water hardness is unlikely to play a significant role in recurrence risk
* Urine dilution significantly decreases urinary activity product ratio of CaP, Caox, monosodiumurate
Proteins:-
Renal stone formation increases with increased protein intake.Addition of 75 gram protein to diet increases urinary calcium excretion by 100 mg. Stone formers more sensitive to calciuric effects of protein consumption than normal subjects.
Calcium:-
Levels of calcium intake above 800 mg recommended are beneficial.Supplemental calcium to be protective be given with a meal (binds dietary oxalate) or combined calcium + estrogen in postmenopausal women does not increase stone risk.
Oxalate:-
Less than 10-15% of urinary oxalate derived from dietary sources
Oxalate(mg/100gm)
Spinach——————–530
Cocoa———————–625
Tea leaves—————-375
Nuts———————–200–600
Though restricted oxalate intake may be given to patients with recurrent nephrolithiasis, a low oxalate diet is most useful in patients with enteric hyperoxaluria, those with underlying bowel abnormalities.
Vitamin C in large doses may increase risks of stone recurrence. Doses should be limited to 2g/day.
Sodium and Potassium:-
High sodium (salt) intake and low potassium intake promote stone formation. The simple solution to prevent stone formation is a low sodium chloride diet (2 gm or less daily) & potassium supplementation via increased intake of fruits & vegetables or by potassium citrate.
Fibre:-
Dietary fibre can influence excretion of ions involved in stone formation by shortening intestinal transit time. A four-five fold increase in fibre intake produces a 20% decrease in intestinal transit time with a concomitant decrease in urinary oxalate excretion. Wheat brans & brans from other cereal grains rich in oxalate have been used to bind calcium in intestine & decrease its absorption. But an increase in oxalate excretion accompanies desired decrease in calcium levels. Alkali provided by vegetable fibre augments citrate excretion
Patients on low-protein, low salt, moderate or low Ca diet had 50% reduction in stone events than those on low-Ca diet alone
Ideal dietary recommendations and controlled dietary regimen to prevent stone formation includes—100 meq Na, 800 mg Ca, 0.8gm/Kg protein, 2200 Kcal/day.
(The author is presently working as Consultant Urologist in Superspeciality Hospital, Govt. Medical College, Jammu)

